Introduction: Pandemic Crisis in the Era of Climate Crisis
Despite the development and distribution of vaccines, the spread of novel coronavirus infections (COVID-19 or SARS-CoV-2) is still raging across the globe with the emergence of variants. When the first case of COVID-19 infection appeared in South Korea in January 2020, the emerging infectious disease (EID) was compared to the previous cases of Severe Acute Respiratory Syndrome (SARS-CoV-1) in 2003 or Middle East Respiratory Syndrome (MERS) in 2015 and so many people expected that the spread would end within a short period of time. However, as of October 2021, the COVID-19 pandemic still continues with approximately 230 million infectees and more than 4.8 million deaths worldwide.
Facing the crisis of the COVID-19 pandemic, climate change is also drawing attention as a major variable that affects the outbreak and spread of infectious diseases. In particular, after the introduction of empirical studies on the correlation between the emergence of COVID-19 and climate change, the public’s interest is growing even more. It may be desirable that public attention to climate change, which could be more serious than any other global crises, is raised even through the COVID-19 pandemic crisis. However, media reports or environmental activists’ hasty conclusion based on insufficient evidence and limited empirical studies that climate change is the major cause of the emergence of COVID-19 pandemic is worrisome in that it could reduce the nature of complex correlation between the two threats to simple and direct causal relations. Studies that have recently drawn public attention to the link between the two global crises are meaningful as an academic effort to understand the devastating knock-on effects of climate change on other crises, rather than actually identifying the cause of the pandemic.
Climate change is a megatrend-type threat that occurs everywhere and affects everything in the atmosphere and the surface of the earth, in which humans and ecosystems live. Climate change poses various unprecedented environmental crises to human living conditions such as sea level rise and extreme weather events. In addition, it has been perceived as a “threat multiplier” that directly or indirectly affects other global threats, including infectious disease outbreaks, food and water insecurity, biodiversity loss, and involuntary displacement. Considering the connection between climate change and infectious disease outbreaks, climate change on the Korean Peninsula has already produced some environmental conditions that could be favorable to unfamiliar infectious diseases from abroad or could make the Korean Peninsula a birthplace for new or variant infectious diseases. While overcoming the ongoing COVID-19 pandemic is a top priority for all of us, we must build national capacity to respond more quickly and effectively to new infectious diseases that will emerge from their coevolution with humanity.
Is Climate Change a Major Cause for the COVID-19 Pandemic?
Earlier this year, many media outlets carried articles with headlines declaring that “the major cause of the spreading Coronavirus (COVID-19) is climate change.” Since the release of the articles, domestic civic groups and environmental activists have been increasing their campaigns to raise public awareness of the correlation between climate change and infectious diseases. In other words, the media provided an opportunity to revive the Koreans’ public interest in the climate change crisis, which might have been underprioritized because of the urgent COVID-19 pandemic. In fact, public interest in the correlation between climate change and COVID-19 was all based on one empirical study, titled “Shifts in global bat diversity suggest a possible role of climate change in the emergence of SARS-CoV-1 and SARS-CoV-2,” which was published by Robert M. Beyer, Andrea Manica, and Camilo Mora in February 2021.1
The study, which links the cause of the COIVD-19 outbreak to the expansion of habitats for bats (major vectors of various zoonotic coronaviruses), explains that global warming has changed ecological conditions and such change has led to local bat species richness and the geographical expansion of the species. It, thus, concludes that the series of changes in ecosystem and bat habitats in the southern Chinese Yunnan Province, fundamentally triggered by climate change, may have caused coronavirus outbreaks. In particular, it is unclear why this study was reported by the Korean media as if climate change certainly was the major cause of the COVID-19 outbreak, even though the study carefully concluded that “climate change may have been an important factor” in the outbreak.
Above all, Yunnan Province, the target area of the empirical study, is approximately 2,000 kilometers away from the Wuhan area of Hubei Province, i.e., the origin of COVID-19. In addition, the actual contact point for the human race and bats, which is most important in identifying the outbreak origin of zoonoses (or zoonotic diseases), was not explained in the study, but the ecological changes in the species of trees and the habitats of bats in the region were used to infer the possibility of cross-species virus transmission. Possibly, urbanization in the Wuhan region, the Chinese culinary tradition of wildlife consumption, or other variables could be the more direct cause of the outbreak. As with any empirical study, there were many academic criticisms on the limitations of this study by ecologists and pathologists shortly after its release,2 but those have not been introduced to the Korean public at all.
Prior to the Korean media’s interest in the connection between climate change and the COVID-19 outbreak, many Korean media outlets had reported that COVID-19 would have similar patterns to the common seasonal respiratory viruses, which are prevalent in cold and dry winters. Those reports were also based on several empirical studies that had statistically analyzed the correlation between the numbers of COVID-19 infectees and geographical or meteorological variables such as geographical location and local temperature and humidity.3 However, none of these news reports and academic analyses were valid.
Contrary to accumulated medical knowledge and epidemiological experience, it is difficult to determine the nature and causality of emerging infectious diseases (EIDs) including COVID-19 in such a short time after the outbreak. Thus, the possibility of EID pandemics, which do not have any countermeasures such as vaccines or cures in place, has long been warned of as a nontraditional emerging security threat. In order to understand EID pandemics as an emerging security threat that causes social anxiety and nationwide damage, it is necessary to understand the complex correlation between the various factors involved.
The Causality Between Climate Change and Infectious Disease
Warnings about the outbreak and spread of zoonotic infectious diseases as another kind of security crisis influenced by climate change have long been highlighted through studies by experts and scientists including the Intergovernmental Panel on Climate Change (IPCC). Following the IPCC’s Fourth Assessment Report (WGII AR4) of 2007, the IPCC’s Fifth Assessment Report (WGII AR5) also warned of the spread of Vector-Borne Diseases (VBDs) transmitted by infected arthropod species (such as mosquitoes, ticks, triatomine bugs, sandflies and blackflies), rodent species (such as mice, rats, and porcupines), and chiroptera species (bats).4
Along with Water-Borne Diseases (WBDs; such as cholera, diarrhea, typhoid, amebiasis, hepatitis, gastroenteritis, giardiasis, campylobacteriosis, salmonella, shigella, and norovirus), which are intensified by water contamination, human risks to VBDs are fully inferred in considering the connection between humans and ecosystems touched by negative consequences from climate change and environmental degradation. For example, water scarcity caused by climate change will inevitably reduce the purification capacity of water in nature, and thus will increase the possibility of WBD infections, especially in underdeveloped countries with insufficient water supply and storage facilities. In addition to water scarcity or drought intensified by climate change, moisture level rise in the atmosphere caused by global warming will lead to more frequent regional heavy rainfall and increase the likelihood of WBD infections spreading through flooding of infectious agents.
As with the hypothesis of the aforementioned study by Beyer et al. (2021), the inference of the increasing possibility of VBD outbreaks is based primarily on unexpected changes in the global ecological environment resulting from climate change. That is, due to the expansion or change in the habitat environment of humans or infectious disease mediators, the interfaces between their respective living spheres have been expanded more than in the past. It also should be noted that most EIDs are zoonoses. Climate change has caused unexpected changes in the habitat environment of infectious disease vectors, but human habitat expansion through urbanization, deforestation, and other environmental degradations have also increased the possibilities of zoonotic VBDs’ outbreaks by expanding the interfaces between humans and wildlife vectors. In fact, scientists estimate that approximately 60% of EIDs are zoonotic and that approximately 72% originate from wildlife.5
Figure 1. Correlations between Global Crises
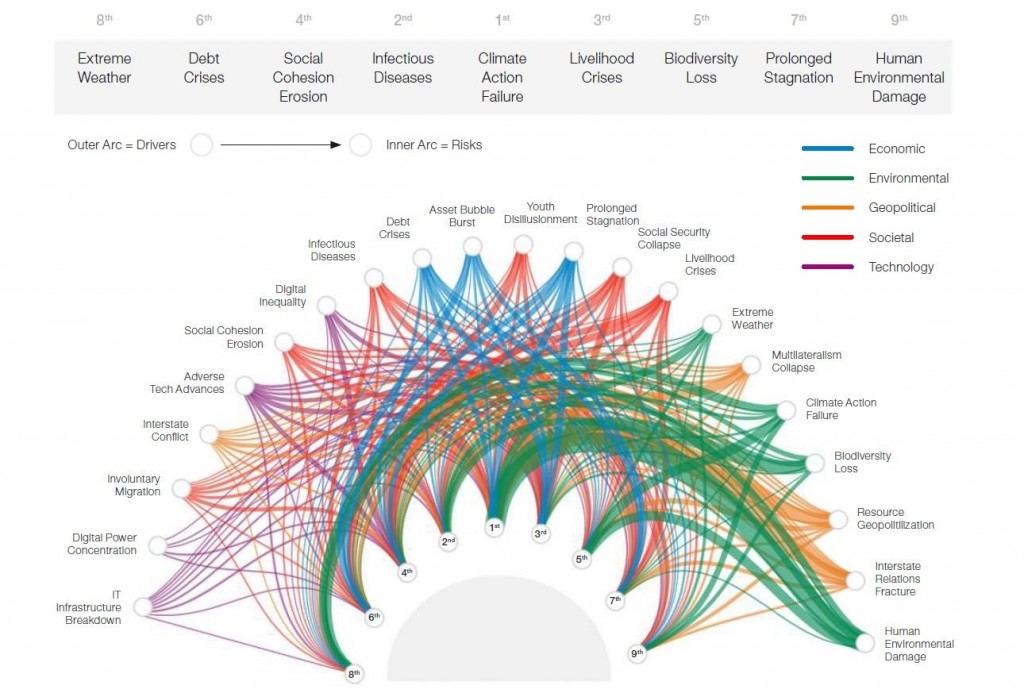
Note: Line thickness illustrates the strength of causality
Source: WEF. The Global Risks Report 2021, p.13.
The causal interactions of variables affecting the emergence of crisis situations, such as pandemics, do not have a unilinear structure. In emerging security areas such as pandemics caused by unknown infectious diseases, the correlation, or reciprocal relationship, of crisis outbreaks is more complex and linked to more variables that should be considered.6 The complex interconnectivity of crises in terms of causality is well illustrated in Figure 1.
Although Figure 1 is based on a survey of more than 840 experts worldwide, rather than on empirical data, it allows us to understand the complexity of causality between crises over global crises in current circumstances or future forecasts. For example, in the case of ‘infectious diseases’ selected as the second most serious global risk following ‘climate action failure’, which has consistently been considered the biggest global risk in recent years, in addition to the climate change factor, environmental factors such as ‘human environmental damage’ and ‘extreme weather’, technological factors such as ‘adverse tech advances’, and social factors such as ‘social security collapse’ are complex causes or drivers, which will possibly initiate or accelerate the emergence of the pandemic crisis.
“Coevolution” of Humanity and Infectious Diseases
With more vaccinated people and the hopeful news of treatment development for COVID-19, prevention and control measures against the new infectious disease are now somewhat accepted as part of daily life. We once had hopes for the so-called “post-coronavirus era”, but we still live with the infectious disease called COVID-19 in the coronavirus era. As a matter of fact, according to the long history of infectious diseases, our expectations for the “post-coronavirus era” are only psychological hopes that will be hardly achieved.
Among the infectious diseases that have emerged throughout human history, only two pathogens—namely, smallpox and rinderpest—have been reported as eradicated, and 99% of polio has been eradicated.7 In other words, mankind is now living in a “post-age” of only three of many infectious diseases that have emerged so far. All of the major infectious diseases that have been prevalent since the 20th century, such as Spanish Flu (H1N1), AIDS, Hong Kong Flu (H3N2), SARS (SARS-CoV-1), Swine Flu (H1N1), MERS (MERS-CoV), Measles virus, Ebola virus, and Zika virus, have not been eradicated and still coexist with mankind. The infectious diseases only have been provisionally eliminated, not eradicated, at the national or regional level through prevention, treatment, and disease control system.
Just as the Spanish Flu (H1N1), which terrorized the world in 1918, brought a pandemic back to humankind again with its variant version called Swine Flu (H1N1) in 2009, most of the infectious diseases that once emerged could mutate and spread again at any time. Our improved health care and disease control systems have successfully kept most infectious diseases from spreading and developing into pandemics, but pathogens are constantly coevolving with their vectors and hosts, namely, humans. Our medical knowledge and technologies on infectious diseases have led us to continuous progress, including the development of vaccines and treatments to respond to the outbreaks, but infectious diseases are also evolving into new species or variants at the same time and neutralizing existing antibodies. In fact, the spread of COVID-19 infection, which has slowed since the introduction of vaccines, is now showing a trend of spreading again due to the emergence of variants. The coevolution of humans and infectious diseases implies that even after the COVID-19 pandemic, other variants or new infectious diseases could emerge and their infectivity or fatality could be much higher than ever.
Climate change is a mega-trend of the present era, which has diverse effects on virtually all human activities, ecosystems, and even the emergence of infectious diseases. It, however, should be noted that the outbreak and spread of various infectious diseases began with the beginning of human history, which was far ahead of the 1990s when the global average CO2 concentration rate in the atmosphere exceeded 350ppm and the loss and damage from climate change became serious as many experts had warned. Although unexpected changes in the ecological environment caused by climate change will affect the outbreak and spread of EIDs, the coevolution between humans and infectious diseases provides an understanding that the emergence of infectious diseases are not the dependent variables of climate change.
Implications for Policy Development
If the habitat environments of vectors such as insects, rodents, and bats, which are transmitting VBD pathogens, have been changing due to climate change, the environment on the Korean Peninsula is not an exception. The public awareness of the interconnectivity between climate change and infectious diseases triggered by the COVID-19 pandemic will be meaningful only when it is developed into a national capacity to suppress or minimize the outbreak and spread of new infectious diseases that would actually be affected by the destructive consequences of climate change.
The Korean Peninsula, which originally belongs to the temperate monsoon climate zone, is gradually changing into a region with sub-tropical characteristics in terms of annual average temperature and precipitation, and accordingly the ecological environments and the types of animals and plants living in it are also changing. In Jeju Island and other sub-tropicalized regions of the southern Korean Peninsula, new ecological environments that were not seen 30 years ago, such as the influx of tropical fishes and the cultivation of tropical fruits, are already being created.
More research is needed to understand how climate change on the Korean Peninsula affects the influx of new infectious diseases from abroad as well as changes in its endemic diseases. More policy attention should also be paid to preparing for and preventing the emergence of new infectious diseases. Because of climate change, more VBDs, especially mosquito-borne infectious diseases such as yellow fever, dengue fever, West Nile fever, Chikungunya fever, and Zika virus, which used to be considered as tropical endemic diseases by Koreans, are more likely to spread on the Korean Peninsula, and bird-borne infectious diseases, i.e., Avian Influenza Viruses (AIVs), are also expected to spread more frequently.
Until now, mosquito-borne infectious diseases have been managed and controlled very successfully in Korea. However, more research and preemptive policy preparations are needed to prevent or respond to bird-borne infectious diseases that continue to increase in frequency and damage. Avian Influenza Viruses (AIVs), which could be infected by poultry such as ducks and chickens or wild birds such as migratory birds, have not been cross-transmitted to humans except for a few cases including H5Ny avian influenza viruses. However, because most of the EIDs are zoonotic diseases, birds should be regarded as potential vectors for new infectious diseases.
In addition, many scientists and experts in epidemiology expect that it is highly likely to develop into an unprecedented and catastrophic pandemic in the event of an outbreak of fatal AIVs, because the vectors will freely spread pathogens to very distant places across national borders.8 Given that South Korea has many habitats for migratory birds and its poultry industry accounts for the largest portion of the livestock industry, the spread or damage in the event of an emerging infectious disease of AIV will be more disastrous than the case of COVID-19. In addition to preventing the influx of existing infectious diseases from foreign countries, it is necessary to review and prepare for the possibility of new zoonotic infectious diseases that may first originate on the Korean Peninsula. Considering that the origin of COVID-19 was not a forest or natural environment where bats lived, but a wet market in Wuhan, China, where humans and wild animals were in close contact, regulations on slaughtering livestock or wildlife should be more strictly maintained and managed.
Coevolution between humanity and infectious diseases suggests that the awareness of infectious diseases, the improvement of the disease control system, and the development of vaccines and treatments are prior to analyses of the outbreak and spread of infectious diseases facilitated by external variables such as climate change. No matter what new infectious diseases or their variants emerge, human medical and health knowledge will eventually be able to overcome by developing vaccines and treatments. However, the COVID-19 pandemic has left a lesson that the development of vaccines and treatments that begin after the emergence of new infectious diseases may be too late to prevent the enormous loss and damage caused by the pandemic. Even though it is impossible to predict what kinds of new infectious diseases will emerge, the national capacity and disease control system to quickly develop countermeasures to respond to the EIDs should be reevaluated and prioritized at the level of national security.
In the early days of the COVID-19 pandemic, South Korea’s disease control system was referred to as an exemplary case of the world. This was not because a new response system or vaccination policies were promptly established, but because the advanced disease control system, which could be set up through the experience of the MERS crisis in 2015, worked effectively and the public’s awareness of personal hygiene was higher than in other countries. The experience of the COVID-19 pandemic leaves a lesson on the importance and necessity of a “social distancing plan” in which all members of society must participate in response to the emergence of infectious diseases. Since it is directly related to the economic life of all citizens, it still remains a policy task to establish social consensus on the effective standard operating procedure of the social distancing plan in South Korea.
Conclusion
It has been more than a year and half since the emergence of COVID-19 around the world, but there are still no cases of successful herd immunity at home and abroad. As of August 2021, the number of infectees worldwide has not decreased due to the emergence of highly contagious ‘Delta’ or ‘Lambda’ variants of COVID-19. For now, the national goal is to secure a vaccination completion rate of more than 70%, which is the primary task of herd immunity. In the end, the time will come when the spread and infection of the virus is eliminated, although it will not be fundamentally eradicated any time soon. The experience and knowledge gained from our experience of the COVID-19 pandemic must be reflected in relevant policies and regulations in order to respond more efficiently and rapidly to new EIDs in the future.
Early studies and media reports on the correlation between climate change and the outbreak of COVID-19 pandemic are of greater significance in that they attracted public awareness of the fact that the climate change crisis could facilitate the emergence of the other kinds of crises such as pandemics. Also, still facing the COVID-19 pandemic, the public’s interest in the correlation between the emergence of new infectious diseases and other promising factors, including climate change, reflects our desire and efforts to minimize the possibility of emerging new infectious diseases in the future. It would be impossible to completely block the outbreak of new infectious diseases. However, as the COVID-19 experience has sufficiently confirmed the importance of developing vaccines and treatments to respond to EIDs, policy support in the research and development of vaccines and treatments must be expanded to prepare national capacities to produce valid countermeasures promptly when a new infectious disease emerges.
The facts that all individuals around the world would be subject to the threats, that the traditional concept for a role of states in terms of political and economic characteristics would be inappropriate to solve and understand the threats, that the nature of the threats could be unclear and unable to defined, that the beginning and end of the threats would be unclear, and that we have limited knowledge and experience make it difficult for us to understand and respond to emerging security threats such as climate change and pandemics. It is urgent to solve the ongoing problem by eliminating the spread of COVID-19, but research and analysis of how our environmental changes caused by climate change have affected and are affecting other global threats should be continued afterwards.
This article is an English Summary of Asan Issue Brief (2021-27).
(‘기후변화와 COVID-19 팬데믹 위기의 연계성에 대한 이해와 시사점’, http://www.asaninst.org/?p=81321)
- 1. Beyer, Robert M., Manica A and Mora C. 2021. Shifts in global bat diversity suggest a possible role of climate change in the emergence of SARS-CoV-1 and SARS-CoV- 2.” Science of the Total Environment, 767 (www.sciencedirect.com/science/article/abs/pii/S0048969721004812).
- 2. “Scientists skeptical of new bat study linking climate change to Covid-19 emergence.” Carbon Brief. February 5, 2021 (www.carbonbrief.org/scientists-sceptical-of-new-bat-study-linking-climate-change-to-covid-19-emergence).
- 3. Sajadi, Mohammad M. et al. 2020. “Temperature, Humidity, and Latitude Analysis to Estimate Potential Spread and Seasonality of Coronavirus Disease 2019 (COVID-19).” JAMA Network Open. 2020; 3(6):e2011834 (https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2767010); Wu, Yu et al. 2020. “Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries.” Science of the Total Environment, 729 (www.sciencedirect.com/ science/article/pii/S0048969720325687); Ahlawat, A., Wiedensohler, A. and Mishra, S.K. 2020. “An Overview on the Role of Relative Humidity in Airborne Transmission of SARS-CoV-2 in Indoor Environments.” Aerosol Air Qual. Res. 20: pp. 1856–1861.
- 4. IPCC. 2007. Climate Change 2007: Impacts, Adaptation, and Vulnerability; IPCC. 2014. Climate Change 2014: Impacts, Adaptation, and Vulnerability (https://archive.ipcc.ch/).
- 5. CRS (Congressional Research Service). 2021. “Wildlife Trade, COVID-19, and Other Zoonotic Diseases.” February 19, 2021 (https://crsreports.congress.gov/product/pdf/IF/IF11494).
- 6. Sangbae Kim. 2016. “Emerging Security and Meta-governance: Theoretical Understanding of the New Security Paradigms.” Korean Political Science Association Journal, 50 (1), pp. 75-104.
- 7. WHO. 2021. “Smallpox Eradication.” Reports by the Director-General: Progress Reports A74/43 (www.who.int/publications/i/item/a74-43—report-by-the-director-general—smallpox-eradication); Roser, Max et al. “Eradication of Diseases.” 2014. Our World in Data (https://ourworldindata.org/ eradication-of-diseases).
- 8. “The Next Pandemic: H5N1 and H7N9 Influenza?” Gavi: The Vaccine Alliance, March 26, 2021 (www.gavi.org/vaccineswork/next-pandemic/h5n1-and-h7n9-influenza); Horimoto, Taisuke and Kawaoka, Yoshihiro. 2001. “Pandemic Threat Posed by Avian Influenza A Viruses.” Clinical Microbiology Review, 14(1): 129-149; Mittal, Niti and Medhi, Bikash. 2007. “The Bird Flu: A New Emerging Pandemic Threat and Its Pharmacological Intervention.” International Journal of Health Sciences, 1(2): 277-283.

 Facebook
Facebook Twitter
Twitter